 May 26, 2020
May 26, 2020The Northern Health Respiratory Department has launched a specialist ambulatory pleural service as part of its Pleural Medicine Unit – the only formalised service of its kind in Victoria.
Pleural diseases occur when there is a problem in the chest cavity, the space between the lung and the chest wall. This often results in the production of fluid in the chest cavity (called pleural effusion) which can lead to breathlessness, chest pain and other symptoms. Fluid in the chest cavity may become infected (called empyema/pleural infection) and air from the lung may sometimes escape in to the chest cavity (called pneumothorax). Pleural diseases are common and the burden is increasing.
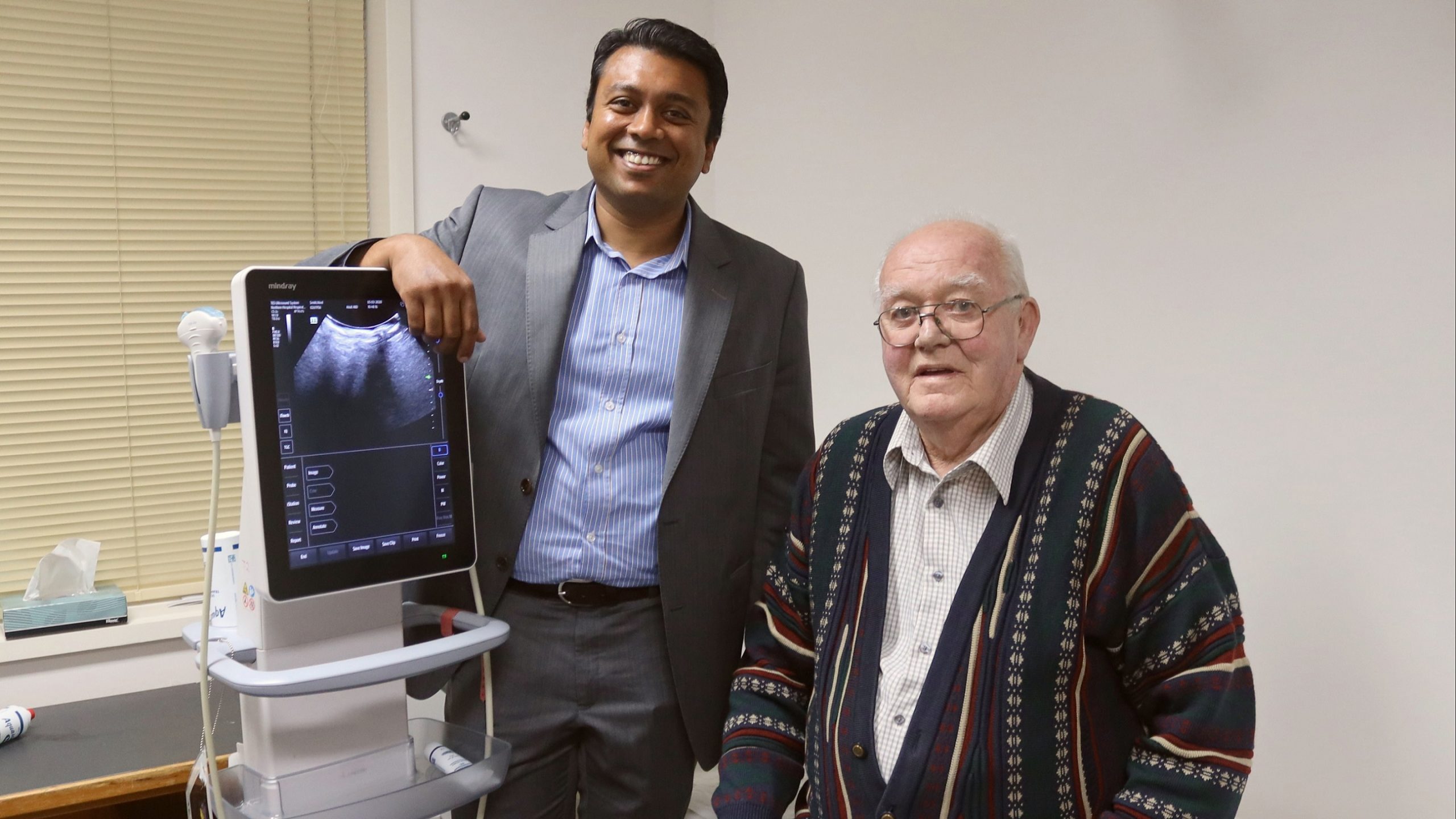
Dr Sanjeevan Muruganandan is a lung specialist and pleural lead, who has done his PhD with Professor Gary Lee in Western Australia – a world leading pleural researcher. The purpose of the Pleural Medicine Unit is to optimise care in patients with pleural diseases by reducing procedures, hospitalisation and standardising care pathways.
“There are over 50 recognised causes of pleural effusion, and our approach is to provide a service that accurately and quickly diagnoses the cause of the pleural problem so that the appropriate treatment can be given.”
“The aim of this innovative service is to reduce further procedures and pleural related hospitalisation, work collaboratively with our thoracic surgical colleagues and ultimately standardise care in all aspects of pleural diseases. In some patients who aren’t fit for surgery, the service offers a less invasive option, which is evidence based,” Dr Muruganandan said.
For example, an indwelling pleural catheter (IPC) can be inserted by the team to assist in the management of chronic recurrent pleural effusion, allowing patients to drain away the fluid whenever they have symptoms, such as shortness of breath. This prevents them from having multiple procedures, prolonged and further hospitalisation.
Noel Smith was one of their patients who had an IPC inserted.
“It meant a lot to me because I was able to be awake while they were doing it and it wasn’t painful. They explained to me what they were doing and it gives you hope if you know what’s going on – especially when you’re awake – I just thought that was tremendous,” Noel said.
“My quality of life definitely improved once I had the catheter in – it helped to take the fluid off, so I was breathing much better. Confidence-wise too, I thought the way they treated me and explained things to me – it built my confidence up so much,” Noel added.
The service is especially unique as it has the first Pleural Clinical Nurse Consultant in Victoria – Kirstin Tirant. Kirstin acts as a direct contact for patients as well as nursing staff when they need assistance, helping them over the phone and reducing the need for patients to have to present to hospital. With the addition of Dr David Feng earlier this year as the Pleural Fellow, the service is growing rapidly and contributing to research in this field.
“For patients with cancer, it’s often more about treating the pleural effusion. Some patients have a very short life-span, so we try to improve their symptoms and quality of life by helping them stay at home for as long as they can by offering that support system,” Dr Muruganandan said.
The team is able to fast-track patients to the pleural clinic, avoiding presenting to the emergency department.
“We have a consult service for the hospital which helps expedite their management plan,” Kirstin said.
“Our team is often involved at the beginning, helping to provide a diagnosis, and we support them throughout their journey. As a team being present throughout their whole journey, we can link these patients with the correct service at the right time,” Kirstin added.

Featured Image: Dr Sanjeevan Muruganandan and patient Noel Smith


